Why Mona?
In a single high-quality device, Mona supports doctors and nurses from patient admission to discharge.
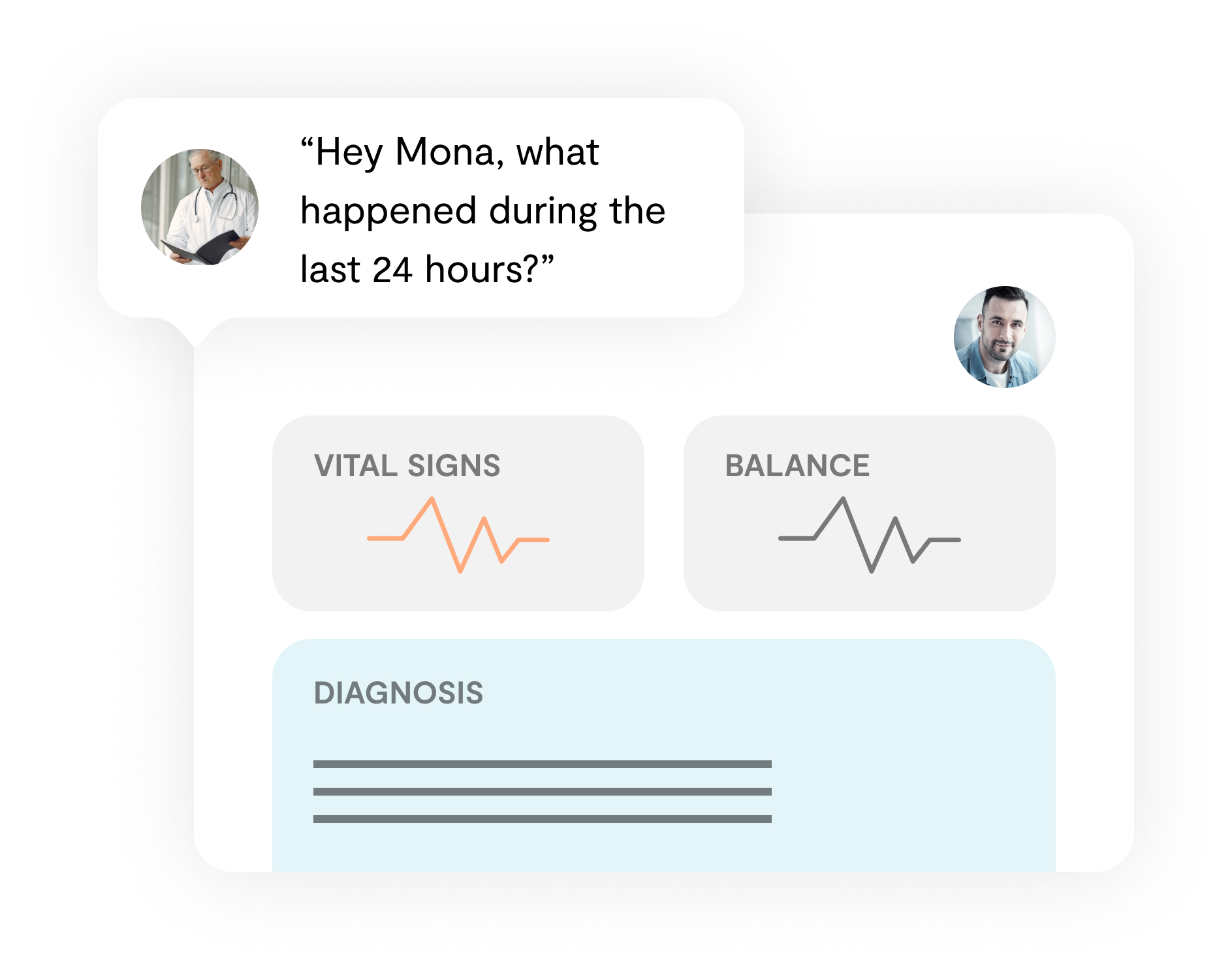
The well-structured user interface enables clinicians to get a good overview of the patient’s condition.
Mona keeps track of all clinical measures and significantly reduces the documentation workload.
Telemedicine – TeleICU
Enables clinicians to securely perform telemedicine through an encrypted audio-video connection, enabling specialist care at the patient bed. No specialized hardware is required.


“Their new technology can be lifesaving for patients, which do not live near big city centres. We are happy to support Clinomic.”
Dr. Florian Reuther, Director of the Association of Private Health Insurance (PKV)


Patient Data Management System (PDMS)
An intuitive and intelligent PDMS enables clinicians to quickly get a concise overview over a patient’s course during a defined timeframe, taking into account individual disease progression.


More Features
- Enables clinicians to accurately document patient data
- Including drugs given, clinical measurements, observation, or procedures
- Provides a simple and efficient way to keep track of common ICU checklists (e.g. FAST-HUG)
- Automatically filling known data from the database
- Reducing the amount of information shown and avoiding confusion about the status of workflows
The Mona Hardware
High-Speed Artificial Intelligence chipset by NVIDIA
Enables ultra-low latency processing of algorithms on premise
Artificial Intelligence powered eight microphone array
For crystal clear audio and telemedicine
60 Ghz radar and localization chip by Infineon
For the best performance even in low lighting conditions
5G and LTE mobile connectivity
For excellent connectivity at all times
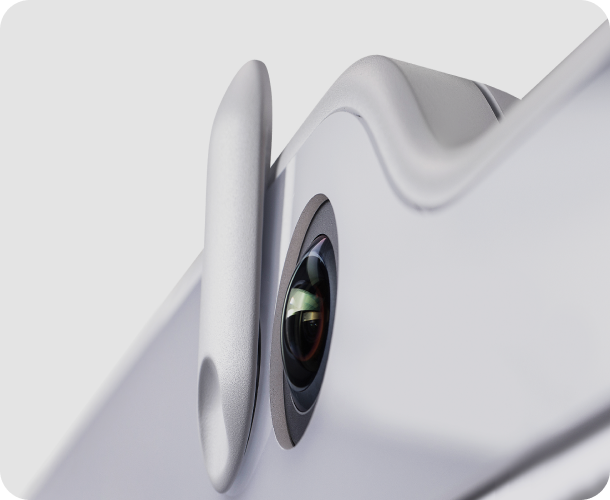
180 degree 4K telemedicine camera
To provide the full view during telemedicine
Book a free Mona demonstration
Book a free 30 minute demonstration via video call, experience a live telemedicine session and discuss all your questions
On-premise or hosted by us
Mona can be hosted either on-premise within your hospital or managed completely by us within our highly secure Clinomic Health Cloud
“Without a doubt, the Mona device is a breakthrough in the care of all critically ill patients.”
Univ.-Prof. Dr. med. Gernot Marx, FRCA


Frequently Asked Questions
So, what’s the problem in Intensive Care?
Intensive Care Medicine is the heart and critical component of hospitals, accounting for 20-25% of hospital resources. Many surgical and non-surgical advances within the last 4 decades are rooted and closely connected to the development in Intensive Care Medicine.
Furthermore, providing high-quality intensive care ensures not only survival but also the quality of the saved life. The ageing society and arising healthcare crises, such as the 2020 coronavirus pandemic, are leading to a drastically increased demand for intensive care beds worldwide. In addition, the number of qualified specialists often does not cover the demand. Today, only 47% of hospitals have the recommended coverage of intensive care specialists and they are unevenly distributed between centers and peripheries. The demand for Intensive Care Medicine is expected to double by 2030. The quality of provided intensive care highly impacts the cost burden on global healthcare systems and economy in general. Drastrically increased data density leads to an increased amount of treatment errors. The Society of Critical Care Medicine reports an average estimated cost of $10,000/day in an ICU. Errors generate costs up to $49 billion per year from preventable medical errors.
Why do hospitals need Mona?
Medical knowledge and health data volume double every three years. Complexity of accurate, evidence-based medicine increases steadily. At the same time, healthcare workers spend 50% of their time in front of computer screens, instead of spending it with their patients. This is even reinforced by economic restrictions and increasing documentation duties, which result in a steadily intensifying workload and rising costs for the hospitals. Notably, relevant patient data is often covered under a layer of irrelevant noise data. Most of today’s medical software relies on static rules – instead of dynamic, case-specific algorithms. This leads to an erroneous user experience and alarm fatigue.
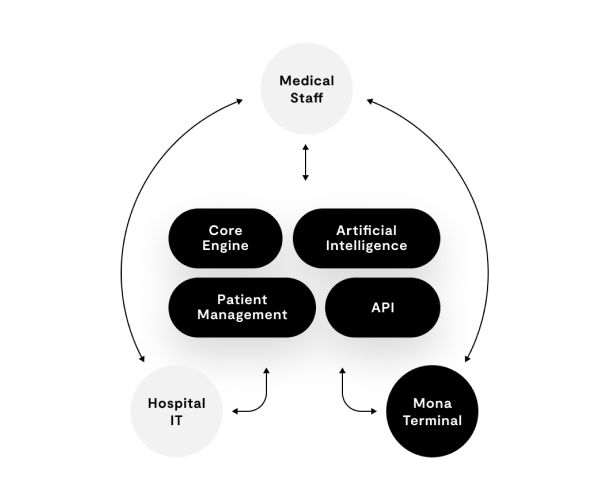
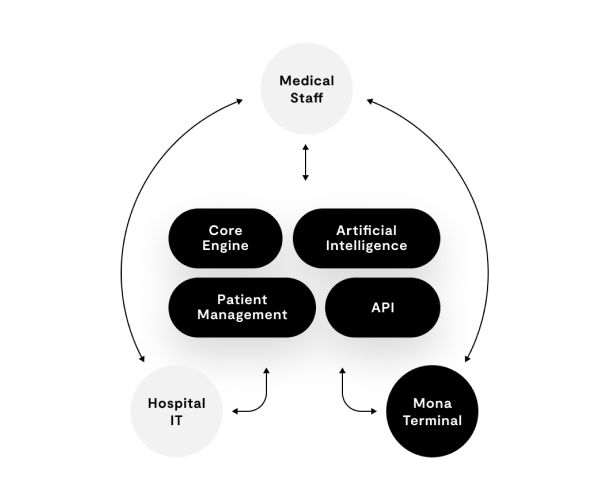
We need to find a better way to deliver the crucial information to clinicians at the point of care. We established a multidisciplinary team of clinicians, researchers, and experts in clinical informatics to design Mona, a smart digital physician assistant for your daily clinical duties at the patient bed. She helps you with documentation, patient data insights and accurate patient treatment. Mona communicates in natural language and helps you to free space for what matters most: time with patients and their relatives.
Is Mona another telemedicine device?
Short answer: No. Mona provides advanced, state-of-the-art telemedicine as one core module.
Mona is the first integrated hardware-software platform, specialized for the intensive care domain. The hardware terminal is equipped with state-of the art technology, such as a 5G Module, radar sensors and artificial intelligence chips from NVIDIA. The system is independent from the hospital’s infrastructure and enables highly encrypted telemedicine, even when network connectivity (e.g. wireless connection) is not optimal. A specialized high-resolution fisheye camera enables crystal clear 180° degree vision, so you can see both the patient and the caregiver, giving you a more complete picture of the situation. 8 microphones enable loud and clear sound, even in noisy environments.
Telemedicine has emerged as a key technology to bring high-level medical care to patients. Multiple studies have shown that providing a dedicated intensivist at an ICU leads to a significant reduction in mortality and reduces the length of stay. Worldwide, telemedical tools have been rapidly adopted to the intensive care setting, providing specialist telemedical guidance to remote hospitals. In the area of acute care medicine, specifically intensive care medicine, telemedicine has proven to be a success story. As a result of the worldwide shortage of medical professionals, not all patients are treated under the supervision of a specialized doctor. Although, it is estimated that, if specialized ICU physician staffing was implemented in nonrural US hospitals, approximately 53,000 lives and US $5.4 billion would be saved annually; as of 2010, only 10%-15% of the US ICUs were able to provide intensive care, clearly a resource urgently needed in response to the coronavirus disease (COVID-19).
The advantages in the reduction of distance barriers between patients and physicians are also used to improve access to high-level intensive care in otherwise medically underserved areas. In adult intensive care wards, the introduction of telemedical surveillance by a specialized intensive reduced severity-adjusted mortality by 33% and 30%, and the incidence of ICU complications by 44% and 50% in two intervention periods in an observational time series cohort study.
Numerous worldwide experiences have shown that the formation of “telemedical excellence centers” is an efficient and fast way to provide telemedical specialist care to large populations. This is especially true for the reaction to global crises such as the coronavirus pandemic, as these telemedical centers can be created rapidly, concentrate specialist care locally, and deliver the highest quality care within large regions without travel restrictions or risk of infection for medical staff.
What about privacy?
Mona has been designed with the highest focus on privacy and security. With Mona, no data ever leaves your hospital. No cloud services, no third party APIs. Mona runs entirely on your own hospital infrastructure (on premise).
Further, we are Health Insurance Portability and Accountability Act (HIPAA) compliant.
All software is developed under the following norms and standards:
- ISO 14971 – Risk management
- IEC 62304 – Software lifecycle management
- IEC 62366-1 Usability
- IEC 60601-1 Electric safety
- IEC 60601-2 Electromagnetic safety
Do you have any more questions?
Contact us!